In today’s always-on world, managing stress isn’t just a luxury—it’s a survival skill. From hormone spikes to mood swings, the impact of stress is deeply woven into our biology. Whether you’re a high-achieving adult, a calm person navigating chaos, or a short person fighting stereotypes and social stress, your body and brain constantly adapt.
This article explores the science of stress and hormones, practical coping strategies, and surprising truths about how we internalize and respond to pressure. We’ll break down essential facts management, discuss how behavioral health plays out in kids and adults, and unpack phrases like get over yourself meaning in the context of emotional growth. You’ll also see how platforms like React Health are changing the game for stress tracking, and why your body might be screaming, “my body is ready” when you least expect it.
Let’s dive into the hormone-stress connection and reclaim your inner calm.
The Science Behind Stress: Hormones That React and Rule
Stress is more than just a mental state—it’s a hormonal chain reaction that affects your sleep, weight, mood, immunity, and even how you age. Your body doesn’t just “feel” stress; it biochemically prepares to survive it.
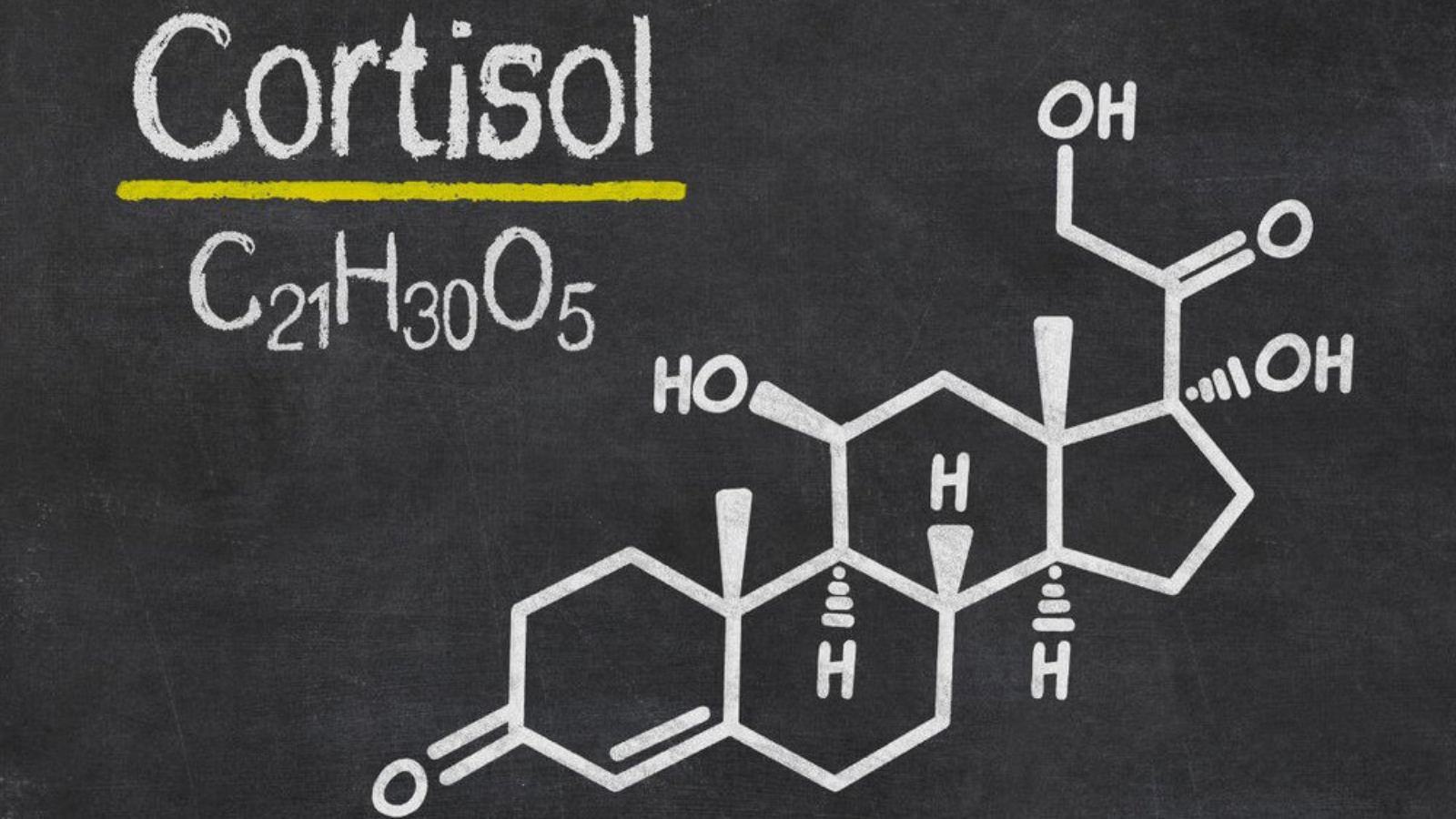
Cortisol: The Commander Hormone
Cortisol, often called the “stress hormone,” is released by your adrenal glands in response to perceived threats—whether physical (like injury) or psychological (like deadlines). Short-term, cortisol can be helpful. It boosts alertness, mobilizes energy, and sharpens focus.
But chronic stress keeps cortisol levels elevated, which can lead to:
- Weight gain (especially abdominal)
- Anxiety and irritability
- Hormonal imbalances (especially in women)
- Weakened immune function
- Poor sleep
Adrenaline: The Short Fuse
When you say “my body is ready”, adrenaline is usually already flowing. It’s responsible for the “fight or flight” response. Your heart races, breathing quickens, and muscles tense. While helpful during emergencies, long-term adrenaline dominance wears your body out.
Estrogen, Testosterone, and Stress
Both estrogen and testosterone are disrupted by chronic stress. In men, lower testosterone may lead to fatigue, loss of muscle mass, and low libido. In women, stress can cause irregular cycles, mood changes, and exacerbated PMS.
Understanding these hormone responses is the first step in facts management—knowing what’s really happening in your body instead of guessing or self-blaming.
React Health and Real-Time Stress Tracking
Thanks to modern tech, we can now track our stress levels in real time. Tools like React Health devices measure key indicators such as:
- Heart rate variability (HRV)
- Sleep cycles
- Skin temperature
- Respiratory rate
These metrics give you a better understanding of how your nervous system reacts to stressors and whether your recovery patterns are strong or weak. This is where facts management comes in—objectively seeing how your body reacts, not just how you feel.
For instance, you might feel calm but have poor HRV, which means your body is under hidden stress. Or you may feel agitated but have solid recovery metrics, indicating you’re more resilient than you think.
Behavioral Health in Kids: Teaching Calm From the Start
One of the most promising areas in stress science is early intervention. Programs focused on calm person kids behavioral health are proving that emotional regulation can be taught—just like reading or math.
When children learn mindfulness, emotion labeling, and coping techniques, it affects hormone development, especially in stress-prone systems.
Benefits of behavioral health education in children:
- Better attention spans
- Lower aggression
- More empathy
- Stronger friendships
- Healthier hormonal responses to adversity
These kids grow into adults who don’t need to “get over themselves”—because they’ve been taught from an early age how to navigate emotions with grace.
Get Over Yourself Meaning: Reframing Emotional Resistance
Let’s talk about the phrase “get over yourself.” Often said dismissively, it’s used to tell someone to stop being dramatic, self-centered, or sensitive.
But the real get over yourself meaning—in the context of stress and hormone science—should be reframed as:
“Learn to separate your emotional identity from your hormonal reaction.”
That’s not dismissive—it’s empowering.
Here’s how:
- You are not your cortisol spikes.
Recognize that stress chemistry is real, but it’s not your whole personality. - You can pause before reacting.
Hormones push for a fast response. Mindfulness slows you down. - You can train new responses.
Emotional regulation isn’t just willpower—it’s a skill, strengthened with practice.
Understanding this helps you become the calm person who handles triggers with intelligence, not suppression.
Short Person Stress: Small Frame, Big Pressure
You might be surprised to learn that body size can influence perceived stress and even hormone balance. For a short person, societal biases can subtly affect cortisol levels and confidence.
Height and Hormonal Confidence
Research has shown that height correlates with perceived authority, particularly in professional settings. This can mean that shorter individuals may unconsciously overcompensate—pushing themselves harder, internalizing more stress, and struggling with imposter syndrome.
Here’s what a short person should know about hormonal health:
- Posture affects hormone levels. Standing tall increases testosterone and lowers cortisol.
- Daily micro-stressors (like being underestimated or overlooked) add up.
- Muscle mass training can help raise confidence-related hormones, regardless of height.
Everyone deserves to feel empowered—your stress load shouldn’t be heavier just because you’re not taller.
Nivel Parts: Stress in the Nervous System
You may have heard of the nivel parts in therapeutic contexts—these refer to subtle inner “parts” of the psyche that develop to protect us during stress. It’s a concept similar to Internal Family Systems therapy, where each part has a voice and a job.
Stress activates different nivel parts, such as:
- The perfectionist (who pushes for results)
- The inner critic (who shames for mistakes)
- The people-pleaser (who avoids conflict)
- The detached observer (who numbs feelings)
These parts form in response to stress and shape hormonal reactions over time. Recognizing which “part” is reacting helps you separate self from stress—another key aspect of facts management.
Building the “My Body Is Ready” Response—Without Burnout
There’s a difference between healthy readiness and stress-induced hypervigilance. When you feel like “my body is ready,” are you:
- Prepared, energized, and grounded?
or - Tense, wired, and anxious?
True readiness comes from hormonal balance—not caffeine, fear, or urgency.
Tips for True Readiness:
- Balance blood sugar
Spikes and crashes in glucose mimic anxiety and affect cortisol levels. - Sleep deeply
Quality sleep restores hormonal rhythms and reduces baseline stress. - Move daily
Exercise releases endorphins and boosts dopamine—a true motivator. - Reflect regularly
Journaling helps process nivel parts and keeps your inner stress team in check.
By combining physiological readiness with emotional regulation, you create a state of calm power—not anxious productivity.
In the next segment, we’ll explore hormone-friendly nutrition, supplement myths, practical grounding techniques, and how to use React Health metrics to create a custom stress-reduction plan. We’ll also revisit social pressures, redefine emotional strength, and offer guidance on teaching resilience to the next generation.
How Nutrition Shapes Hormonal Stress Response
Food is more than fuel—it’s data. What you eat directly informs how your body produces and regulates hormones, especially those involved in stress like cortisol, insulin, and adrenaline. If you’re trying to become more resilient or just feel more balanced, hormone-supportive nutrition is a cornerstone.
The Cortisol Balancing Plate
A balanced meal can help regulate cortisol levels throughout the day. Here’s how to build one:
- Protein (20–30g): Eggs, chicken, lentils, or tofu stabilize blood sugar and boost dopamine production.
- Healthy fats: Avocados, olive oil, nuts support hormonal synthesis.
- Complex carbs: Sweet potatoes, oats, and quinoa reduce cortisol by promoting serotonin.
- Leafy greens: Magnesium-rich veggies like spinach help lower anxiety.
This combination sends the message to your body: my body is ready—in a real, nourished way—not the panicked “ready” that comes from stress-induced hyperactivity.
What to Avoid When You’re Stressed
Stress makes us crave quick fixes—sugar, caffeine, and processed carbs. But these foods spike blood sugar and exacerbate hormonal dysregulation.
Avoid or limit:
- Caffeine overload: Increases cortisol, especially when consumed on an empty stomach.
- Refined sugars: Spike insulin and worsen fatigue once the crash hits.
- Alcohol: Disrupts sleep and cortisol regulation.
This is not about perfection—it’s about facts management. Knowing the effects of certain foods on your hormones helps you make better choices, even when emotions run high.
Supplements for Stress and Hormonal Balance
While food should come first, the right supplements can help manage stress when used appropriately.
Helpful Options:
- Ashwagandha: Lowers cortisol and enhances resilience.
- Magnesium glycinate: Supports muscle relaxation and sleep.
- L-theanine: Found in green tea, it promotes calm focus.
- Omega-3s: Reduce inflammation and improve mood balance.
If you’re using tools like React Health, you can test how these supplements affect your biometric data like HRV and sleep quality.
Using React Health for Personalized Stress Insights
React Health provides real-time data to support your mental and physical well-being. But tech is only as useful as how you apply it.
Key Metrics to Watch:
- Heart Rate Variability (HRV): Low HRV = more stress. Higher HRV = better recovery.
- Resting heart rate: Chronically elevated? Your nervous system is on edge.
- Sleep stages: Lack of deep sleep or REM = impaired hormone repair.
- Breathing patterns: Shallow, erratic breathing is common in stress-prone individuals.
By analyzing these trends, you move from vague feelings to hard facts management—and begin to understand which nivel parts show up during different life stressors.
Grounding Techniques That Actually Work
Forget “just calm down”—you need actionable tools that reset your nervous system and restore balance to your hormones.
1. The 5-4-3-2-1 Technique
Engage your senses to anchor your mind:
- 5 things you can see
- 4 things you can touch
- 3 things you hear
- 2 things you smell
- 1 thing you taste
This method can calm your nivel parts quickly when they’re in “overfunctioning” mode.
2. Box Breathing (Used by Navy SEALs)
- Inhale for 4 seconds
- Hold for 4 seconds
- Exhale for 4 seconds
- Hold for 4 seconds
This activates the parasympathetic nervous system, helping your brain and body realize: my body is ready—not for war, but for recovery.
Redefining Calm: It’s Not the Absence of Stress
Many people think being a calm person means you don’t feel stress. In reality, calmness is the ability to respond, not react. It’s being able to pause, reflect, and choose—even in high-stress situations.
In children, this skill is learned through consistent modeling and behavioral support, like the kind seen in calm person kids behavioral health programs. Adults can learn it too—but it takes unlearning emotional shortcuts like rage, shutdown, or avoidance.
Here’s the modern get over yourself meaning:
Get over the old version of yourself that reacts out of fear.
Step into the self that chooses powerfully—even under pressure.
Hormone Harmony for All Body Types
Let’s address an overlooked point: how hormone balance and stress management vary depending on body composition and genetics. Whether you’re a short person, tall, muscular, lean, or curvy, your endocrine response can be shaped, not doomed.
For Short Individuals:
- Posture and breathing exercises help regulate cortisol.
- Adding resistance training boosts testosterone and confidence.
- Choose foods rich in magnesium and B-vitamins for mood support.
Being a short person does not mean you’re less capable of handling stress—but society’s perception may unintentionally elevate your stress load. Mindful movement and hormonal nutrition can counterbalance that effect.
Understanding Your Nivel Parts to Stop Overreacting
Those inner voices you hear during stress—the perfectionist, the critic, the one who says you’re failing—aren’t flaws. They’re parts of you that developed to keep you safe.
What stress science and behavioral health now tell us is that:
- These nivel parts are not enemies
- They’re protectors, but outdated ones
- You can thank them and lead with your whole self
When you understand what each part fears—rejection, judgment, inadequacy—you can step in as the calm adult and say, “I’ve got this. My body is ready.”
Case Study: Teaching Kids Resilience Early
In schools using calm person kids behavioral health programs, children are taught emotional vocabulary, movement-based regulation (like yoga or dance), and group processing.
Results from these programs include:
- Fewer classroom disruptions
- Improved test scores
- Better peer relationships
- Long-term hormonal benefits (like stable cortisol patterns)
The earlier we normalize emotional flexibility, the better we prepare future adults to handle adversity without burnout.
Practical Routine for Stress & Hormone Reset
Here’s a sample day for rebalancing your hormones and easing chronic stress:
Morning:
- Wake with a glass of warm lemon water
- 15 minutes of light stretching or yoga
- Balanced breakfast: protein + healthy fat + complex carb
- Brief journaling to check in with your nivel parts
Midday:
- Mindful lunch (no screens)
- Walk outside for sunlight and endorphins
- Check React Health for HRV or stress score
Evening:
- Magnesium-rich dinner (leafy greens + salmon + sweet potato)
- Screen detox 1 hour before bed
- Box breathing or meditation
- Express gratitude: one thing that made your body feel “ready” today
Consistency, not perfection, is what rebuilds hormonal strength and stress resilience.
Coming up next: In the final section, we’ll explore myth-busting common misconceptions about stress, how to maintain hormone balance through life changes, and a complete recap of tools you can use daily to stay grounded, energetic, and emotionally strong.
Myth-Busting Stress and Hormones: What You’ve Been Told vs. What’s True
Even in the era of wellness trends and wearable tech, myths about stress and hormones still run rampant. Let’s clear the air and ground ourselves in facts—not fads.
Myth 1: “Stress is all in your head.”
False. Stress is very real—and physical. Hormones like cortisol, adrenaline, and insulin don’t care whether your stress comes from a lion, a deadline, or traffic. They respond all the same. Tools like React Health prove this with data: your heart rate variability drops, your breathing speeds up, and your recovery time suffers.
Myth 2: “Only anxious people are stressed.”
Also false. You can be a calm person on the outside and still carry internal tension that manifests in your digestion, sleep, or skin. It’s about biology, not bravado. That’s why programs like calm person kids behavioral health matter—they teach kids to check inside, not just perform calmness.
Myth 3: “Short people are naturally more high-strung.”
Stereotype alert. A short person may face different social stressors (being underestimated, interrupted, or overlooked), but height has no biological link to emotional resilience. Hormonal balance comes from how you eat, move, sleep, and process—not how tall you are.
So the next time someone says “get over yourself,” reflect on the get over yourself meaning: it’s not about shrinking your experience. It’s about rising above reactive identity and choosing calm, responsive action.
How to Support Hormones Through Life Changes
Hormonal stress responses change dramatically during different phases of life. From adolescence to pregnancy, midlife to menopause or andropause, each stage brings a new internal landscape.
Adolescents & Young Adults
- Hormones surge and fluctuate, increasing emotional reactivity.
- Stress from academic, social, and identity pressures spikes cortisol.
- Facts management tools—like journaling or HRV monitoring—help build awareness.
Pregnancy & Postpartum
- Estrogen and progesterone shifts can cause sleep disruptions and mood changes.
- Social isolation or lack of support amplifies stress.
- Cortisol crosses the placenta, affecting the baby—another reason calm person kids behavioral health starts with parents too.
Midlife (30s–50s)
- Testosterone, estrogen, and DHEA begin to decline.
- Chronic stress shows up more in belly fat, burnout, or emotional numbness.
- Now is the perfect time to build routines that tell your body, “my body is ready”—for recovery, not just performance.
Older Adults
- Cortisol regulation becomes less efficient.
- Sleep and memory decline if stress is unaddressed.
- Prioritizing nutrient-dense foods, community, and light exercise helps maintain hormone balance.
The Role of Identity in Stress Management
Stress isn’t just physiological—it’s deeply personal. Our identity, beliefs, and self-narrative impact how we interpret and respond to stress.
Ask yourself:
- Do I identify as someone who thrives under pressure, or someone always overwhelmed?
- Do I think I deserve rest, or feel guilty slowing down?
- When I feel tension, which nivel parts step in—and why?
Doing this facts management work creates space to shift the narrative. Instead of “I’m just not good with stress,” you can say, “I’m learning new tools to regulate and adapt.”
Social Media, Comparison, and Cortisol
In the digital age, comparison-induced stress is one of the biggest silent saboteurs of hormonal balance. Every scroll exposes you to:
- “Perfect” routines that make you question your own
- Fitness influencers claiming 4 a.m. wake-ups and zero stress
- People shouting “my body is ready” when you feel exhausted
Comparison spikes cortisol and lowers self-esteem. Here’s how to buffer against it:
- Curate your feed like a mood board—only follow accounts that teach or uplift.
- Schedule social media time, and take weekly breaks.
- Use data (like from React Health) to focus on your body’s truth, not someone else’s image.
The Hormone Reset Toolkit: What to Use and When
Let’s round this out with a clear toolkit of daily and weekly habits to keep your stress in check and your hormones in harmony.
Daily Toolkit
| Goal | Action |
|---|---|
| Lower cortisol | 10-minute meditation, magnesium-rich breakfast |
| Improve sleep hormones | Limit caffeine, get sunlight, journal before bed |
| Stabilize insulin | Eat balanced meals (protein, fat, complex carbs) |
| Release trapped tension | Daily movement: yoga, walk, resistance training |
| Calm nivel parts | Box breathing, naming emotions, short voice memos |
Weekly Toolkit
| Goal | Action |
|---|---|
| Track recovery | Use React Health to review HRV and sleep trends |
| Plan for hormone-friendly meals | Batch cook with leafy greens, fatty fish, nuts, and seeds |
| Reconnect socially | Schedule one meaningful conversation or walk with a friend |
| Reflect on self-talk | Ask: “What’s my current identity? Who am I becoming?” |
| Educate | Watch one video or read one article on stress, hormones, or wellness |
Consistency—not intensity—is what shifts your stress response. This is how you teach your body: you’re safe, nourished, and supported.
Teaching the Next Generation Emotional Mastery
Why wait until adulthood to teach stress management? Programs like calm person kids behavioral health are showing that kids who learn these tools early:
- Have lower baseline cortisol
- Perform better academically
- Are more emotionally resilient as adults
If you’re a parent, teacher, or caregiver, integrate emotional vocabulary, mindfulness games, and breathing exercises into daily routines. When kids hear “get over yourself,” they won’t internalize it as shame—they’ll understand it as: regulate, reflect, reset.
Final Thoughts: From Reacting to Responding
Stress is not the enemy. It’s a messenger—a signal from your body that something needs attention. When we ignore it, over-function, or suppress it, we burn out. But when we listen, reflect, and support our hormonal system, we grow.
Let’s review what you’ve learned:
✅ Facts management leads to better decisions and self-awareness
✅ Height, identity, and emotions all impact how stress is internalized
✅ Tools like React Health provide real data to track stress and recovery
✅ You can be a calm person even in chaos—it’s a skill, not a personality type
✅ The get over yourself meaning is about emotional ownership, not suppression
✅ Understanding your nivel parts helps break reactive cycles
✅ Hormonal health is possible at every life stage—with the right routines
So when life gets intense, and stress shows up again (because it will), take a breath and say:
My body is ready.
Ready to listen.
Ready to regulate.
Ready to rise.